Imagine a world where you could share about your mental health challenges with your boss and coworkers, and not worry about side glances, or worse, workplace discrimination, afterward. Where sharing led to compassion and support and brought your team closer together. Where the words “career-limiting move” never crossed your mind. Where you could safely be you.

We live in a culture that has engrained some pretty whack-ass notions of what emotional strength, fragility and success look like. Even when it doesn’t serve us, it often feels less risky to pretend everything is fine, hide what’s hurting us and push through. Mental health is an awkward subject in the workplace.
An organization called The Stability Network is shifting the narrative. It sends out speakers who live with mental health conditions to tell their stories in workplaces around the world, and to demonstrate that it’s possible to have an episode, recover and continue to thrive in all manners and ways. TSN’s tag line says it all: Changing the way we talk about mental health, one story at a time.
Twenty years ago, I took a five-week medical leave from my job because of depression. My immediate teammates were amazingly supportive, but I remember feeling anxious about what the rest of the office thought about my absence, and whether I would retain the respect of my peers when I returned.
On my first day back, I heard many kind greetings, but the reason for my absence was carefully avoided. You know how when someone returns after a surgery or a heart attack, everyone has a similar story to tell? Either theirs, or someone they know? No one had a story to share with me. Stories of mental illness recovery just weren’t the kind of thing people talked about.
Unsurprisingly, I felt shame around my illness. For the next 15 years, I played my mental health cards close to my chest, until I understood that greater power came from speaking the truth. Changes in perception don’t come from statistics and reports, they come from seeing, knowing and hearing from people with lived experience. Discomfort is dispelled when the people with the lived experience make it okay to talk about it. Silence begets more silence.
I’m grateful to The Stability Network for its commitment to creating a space for mental health stories in the workplace, and in partnership with them, I’ve committed to telling mine. As a speaker for TSN, I hope to stand in front of audiences large and small and show that any dodgy vibe from me is completely attributable to the fact that I’m a Pacific Northwesterner who likes neither sushi nor salmon—utter heresy—and not because I live with Complex PTSD and depression.
If you would like to help us create a world where workplaces are supportive of people experiencing mental health challenges by inviting a speaker to yours, you can let me know, or you can click here.
 In December, I turn 50. Along with the ravages that only gravity can inflict comes an acknowledgment: even at the half-century mark, I’m not finished doing the work to emotionally integrate the trauma that happened in my life when I was a kid.
In December, I turn 50. Along with the ravages that only gravity can inflict comes an acknowledgment: even at the half-century mark, I’m not finished doing the work to emotionally integrate the trauma that happened in my life when I was a kid.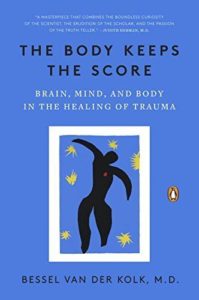 I’m also reading Bessel van der Kolk’s groundbreaking book
I’m also reading Bessel van der Kolk’s groundbreaking book  It’s one sleep since the end of
It’s one sleep since the end of  How ‘bout that gene testing? Is 23andMe setting itself up to be a next-wave health diagnosis and treatment tool? It’s certainly been a discovery process for me, once
How ‘bout that gene testing? Is 23andMe setting itself up to be a next-wave health diagnosis and treatment tool? It’s certainly been a discovery process for me, once  I found a really compelling post from Danielle LaPorte in my inbox yesterday called
I found a really compelling post from Danielle LaPorte in my inbox yesterday called  One thing that strikes me as a large factor in courageous-move-making is TIMING. Sometimes it takes a while – three months, three years – to plan a big change. Sometimes you can only juggle one change at a time, and so other things get backburnered while you replant your feet and get steady (or steadier) again. The key is to keep what you want (to risk or change) on your radar. Don’t backburner it on your neighbor’s stove so that you lose sight of it, and start taking small steps toward it, even if you’re not ready to swing the whole deal.
One thing that strikes me as a large factor in courageous-move-making is TIMING. Sometimes it takes a while – three months, three years – to plan a big change. Sometimes you can only juggle one change at a time, and so other things get backburnered while you replant your feet and get steady (or steadier) again. The key is to keep what you want (to risk or change) on your radar. Don’t backburner it on your neighbor’s stove so that you lose sight of it, and start taking small steps toward it, even if you’re not ready to swing the whole deal. Finally, whatever you decide to do, or not do, when it comes to risk-taking and change, BE TRUE TO YOU. Some people fly on the safe side, and will always do so, and if your feelings are telling you it’s all good, then it’s all good. I remember going through a
Finally, whatever you decide to do, or not do, when it comes to risk-taking and change, BE TRUE TO YOU. Some people fly on the safe side, and will always do so, and if your feelings are telling you it’s all good, then it’s all good. I remember going through a  I haven’t posted much lately, but it’s not just my blog to which my recent rut of doom has extended. Depression doesn’t judge or pick favorites. It squashes everything – gym time, social outings, work motivation, romanticalness and creativity. It asphyxiates joy. It really sucks.
I haven’t posted much lately, but it’s not just my blog to which my recent rut of doom has extended. Depression doesn’t judge or pick favorites. It squashes everything – gym time, social outings, work motivation, romanticalness and creativity. It asphyxiates joy. It really sucks. Now for the depressed writer (I know a lot of you personally): I have an essay about a life-altering encounter that I’ve been working on for years. I wrote the first draft in early 2013. I wrote the second draft in 2014. I finally submitted it in January 2015. It was rejected. I tried news magazines and they said it was too literary. I tried literary magazines and they said it wasn’t deep enough. Last August, I had an editor at one lit mag offer to read it a second time if I made (his suggested) revisions. I gave it a shot; he rejected it again. Some writing friends critiqued the essay and I did more revisions. I submitted it to more places and received more rejections. Then I met the editor in person at a conference, and he offered to read it a third time. I worked on it for another month and sent it off to him, the essay’s twelfth submission in all.
Now for the depressed writer (I know a lot of you personally): I have an essay about a life-altering encounter that I’ve been working on for years. I wrote the first draft in early 2013. I wrote the second draft in 2014. I finally submitted it in January 2015. It was rejected. I tried news magazines and they said it was too literary. I tried literary magazines and they said it wasn’t deep enough. Last August, I had an editor at one lit mag offer to read it a second time if I made (his suggested) revisions. I gave it a shot; he rejected it again. Some writing friends critiqued the essay and I did more revisions. I submitted it to more places and received more rejections. Then I met the editor in person at a conference, and he offered to read it a third time. I worked on it for another month and sent it off to him, the essay’s twelfth submission in all. If you have a peach pit of faith in something, despite the “stated” odds, or a feeling that as crazy as your particular notion seems, it is meant to be, hang on to it. Hang the fuck on. Feed it and stoke it and dress it in a warm, fuzzy kangaroo onesie so it never leaves. Do not give up. Please. To give up on it is to give up on you.
If you have a peach pit of faith in something, despite the “stated” odds, or a feeling that as crazy as your particular notion seems, it is meant to be, hang on to it. Hang the fuck on. Feed it and stoke it and dress it in a warm, fuzzy kangaroo onesie so it never leaves. Do not give up. Please. To give up on it is to give up on you. No matter your political views, news sources and musical tastes, it’s hard to evade the gloom that has descended around the globe. And if you’re predisposed to or are a chronic depression sufferer like me, then these are exceptionally wonky-inducing times. Yes, wonky, which, by the way, encompasses the following:
No matter your political views, news sources and musical tastes, it’s hard to evade the gloom that has descended around the globe. And if you’re predisposed to or are a chronic depression sufferer like me, then these are exceptionally wonky-inducing times. Yes, wonky, which, by the way, encompasses the following: What hump, you ask. Ahhhh. See, this is where I lost track of the bouncing mental health ball myself until last week. The hump is the creep. Whaaaat? (I’m not messing with you, seriously.)
What hump, you ask. Ahhhh. See, this is where I lost track of the bouncing mental health ball myself until last week. The hump is the creep. Whaaaat? (I’m not messing with you, seriously.) Yoga, meditation, healthy food, supplements, exercise: yes, yes, yes, yes. Any other alternative and complementary therapies you use to combat depression: yes, yes, yes, yes. We are warriors, all of us. But even the strongest warrior can only handle so many body blows. Sometimes the most effective and compassionate solution is right in front of us and we don’t see it. And that, in a nutshell, is 2016.
Yoga, meditation, healthy food, supplements, exercise: yes, yes, yes, yes. Any other alternative and complementary therapies you use to combat depression: yes, yes, yes, yes. We are warriors, all of us. But even the strongest warrior can only handle so many body blows. Sometimes the most effective and compassionate solution is right in front of us and we don’t see it. And that, in a nutshell, is 2016. Without fail, each month one of my site’s top search phrases is “when your mother is crazy,” or “how to deal with a crazy mom,” or something similar. (Even more popular is “does strawberry flavor come from beaver butt,” but that’s a whole other story.) It seems like there are a lot of people struggling in their relationship with a mother who has a mental illness, just like I did at one time. I’m writing this post (and stuffing it full of love) for them. For you.
Without fail, each month one of my site’s top search phrases is “when your mother is crazy,” or “how to deal with a crazy mom,” or something similar. (Even more popular is “does strawberry flavor come from beaver butt,” but that’s a whole other story.) It seems like there are a lot of people struggling in their relationship with a mother who has a mental illness, just like I did at one time. I’m writing this post (and stuffing it full of love) for them. For you. You may never get an answer to “what’s wrong with my mom?” and it’s not always black and white anyway. So, that leaves an open question hanging in the air, but it doesn’t have to stop you from living your life and planning your future.
You may never get an answer to “what’s wrong with my mom?” and it’s not always black and white anyway. So, that leaves an open question hanging in the air, but it doesn’t have to stop you from living your life and planning your future.